Unveiling the Silent Struggle: Exploring the Alarming Prevalence of Diabetes in Lower and Middle-Class Neighborhoods in America. In the heart of these communities, a health crisis quietly unfolds, shaping lives and challenging well-being. This blog post delves into the stark reality of diabetes prevalence within lower and middle-class neighborhoods in America. Beyond the statistics lies a nuanced narrative, unraveling the complex intersections of socioeconomic factors and health outcomes. Join us as we navigate through the intricacies of this pressing issue, shedding light on the disparities that demand attention and action.
Unmasking the Diabetes Divide:
A Closer Look at Health Disparities in Lower and Middle-Class American Neighborhoods
The prevalence of diabetes in the United States has witnessed a significant upswing over the past two decades, escalating from 6.4% in 1999−2002 to 9.4% in 2013−2016 among adults aged ≥18 years.[1] In 2018 alone, an estimated 34.1 million adults were reported to have diabetes, with an additional 88 million categorized as having prediabetes.[1]
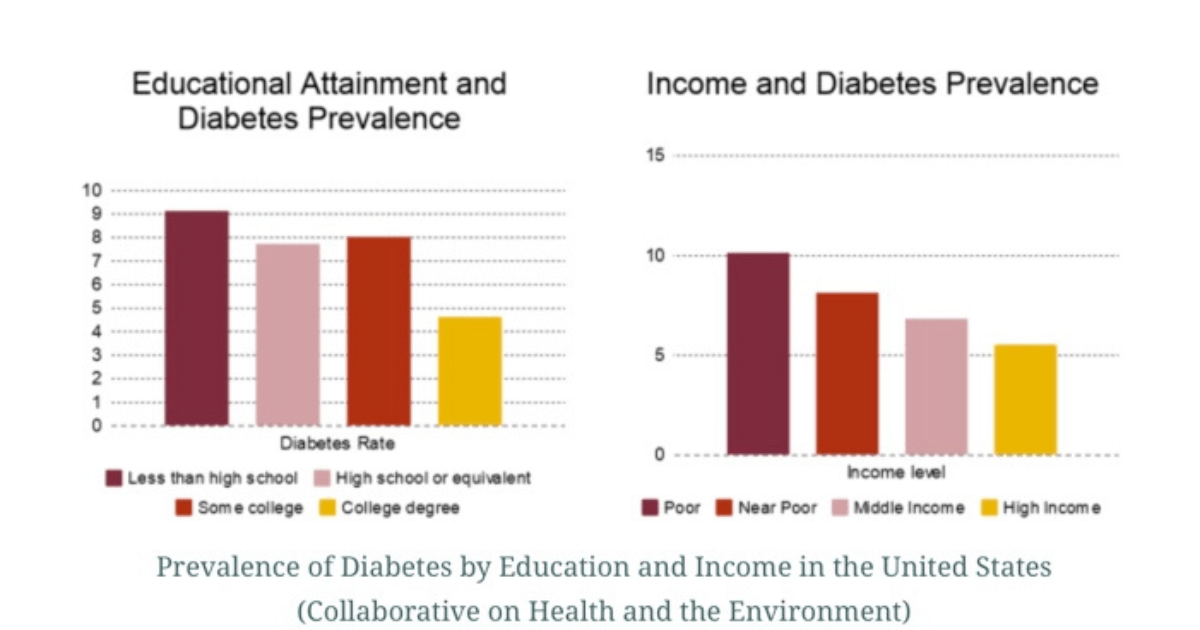
This health burden is not distributed uniformly, with lower-income populations shouldering a disproportionate share, as evident in the staggering relative percentage increase of diabetes prevalence among those classified as middle-income, near-poor, and poor between 2011 and 2014.[1]
Numerous contributing factors underline the income disparities in diabetes, spanning differences in demography, financial resources, healthcare access, environmental conditions, and health-related behaviors[1]
Racial and ethnic minorities, coupled with older adults, experience a higher prevalence of diabetes, concentrating within low-income groups. Additionally, risk factors like obesity and physical inactivity are more prevalent among lower-income populations. Understanding these multifaceted determinants is crucial for developing targeted interventions to address the health inequalities in socioeconomically disadvantaged communities.[1]
[2]
Decoding Diabetes Disparities:
Unveiling the Root Causes
In the realm of public health, diabetes reveals stark disparities, particularly impacting lower-income communities. Unraveling the core causes behind these inequalities is pivotal for crafting effective strategies for prevention and intervention. Below are some of the reasons listed for these disparities:
1. Limited Healthcare Access
Unequal access to healthcare services hinders timely diabetes screenings and management, disproportionately affecting lower-income individuals.[4]
2. Socioeconomic Stressors
Financial strain and unstable living conditions elevate stress levels, fostering unhealthy coping mechanisms that contribute to an increased risk of diabetes.[3]
3. Nutritional Challenges
Scarce access to affordable, nutritious foods in lower-income areas leads to an overconsumption of processed, unhealthy options, amplifying the risk of obesity and diabetes.[3]
4. Environmental Barriers
Lack of safe spaces for physical activity in low-income neighborhoods discourages exercise, a critical factor in the elevated risk of obesity and diabetes.[3]
5. Educational Gaps
Limited educational opportunities and health literacy impede understanding of diabetes prevention, reinforcing disparities in lower-income communities.[4] .
6. Social Determinants
Discrimination and a lack of community support contribute to chronic stress, influencing unhealthy coping mechanisms and diabetes prevalence.[4]
7. Genetic Factors
Genetic predisposition, coupled with limited access to preventative healthcare, contributes to a higher diabetes prevalence in certain lower-income communities.[4]
8. Occupational Hurdles
Lower-income jobs with long hours and irregular schedules make it challenging for individuals to prioritize healthy habits, impacting diabetes risk.[3]

How can we help?
Combatting the diabetes issue among low-income populations requires a multifaceted approach that addresses both systemic and individual factors. Here are several strategies that somebody can implement in society to tackle this health disparity:
1. Accessible Healthcare Services:
-
Increase accessibility to affordable healthcare services, including regular diabetes screenings and preventive care.
-
Establish community health clinics in low-income neighborhoods to provide convenient and comprehensive health services.
2. Health Education Initiatives:
-
Implement targeted health education campaigns focusing on diabetes prevention, healthy lifestyle choices, and the importance of regular check-ups.
-
Collaborate with community organizations and schools to enhance health literacy and promote awareness.
3. Nutritional Support Programs:
-
Introduce initiatives that increase access to affordable, nutritious foods in low-income areas, such as community gardens, farmers' markets, or subsidies for healthy food options.
-
Provide nutritional education to empower individuals to make healthier food choices within budget constraints.
4. Community Wellness Programs:
-
Establish community-based wellness programs that promote physical activity through free or affordable exercise classes, walking groups, or recreational spaces.
-
Encourage local businesses to support employee wellness programs, fostering a culture of health in the workplace.
5. Financial Assistance for Medications:
-
Implement programs to provide financial assistance or subsidies for essential diabetes medications and supplies.
-
Advocate for policies that ensure affordable and equitable access to insulin and other diabetes-related medications.
6. Employment and Economic Support:
-
Advocate for policies that address living wage standards to alleviate financial stressors contributing to diabetes risk.
-
Promote workplace wellness programs that support employees in maintaining healthy lifestyles.
7. School-Based Interventions:
-
Integrate comprehensive health education into school curricula, emphasizing the importance of nutrition, physical activity, and overall well-being.
-
Ensure that school environments provide healthy food options and opportunities for physical activity.
8. Policy Advocacy:
-
Advocate for policy changes that address social determinants of health, such as affordable housing, safe neighborhoods, and reduced exposure to environmental stressors.
-
Collaborate with policymakers to prioritize health equity and integrate diabetes prevention measures into broader public health initiatives.
9. Telehealth Services:
-
Expand access to telehealth services, enabling individuals in low-income communities to receive medical consultations and diabetes management support remotely.
10. Community Engagement and Empowerment:
-
Foster community engagement by involving residents in the development and implementation of health programs.
-
Empower individuals with diabetes through support groups, peer mentorship, and resources that facilitate self-management.

Diabetes-Friendly Meal Plans
Meal Plan 1: Plant-Powered Basics
Breakfast:
- Water, sliced berries, and a sprinkle of chia seeds can be added to oatmeal.
- Almond or soy milk.
Lunch:
- Quinoa salad with canned chickpeas, cherry tomatoes, cucumbers, and a lemon-tahini dressing.
- Whole-grain pita or rice cakes.
Dinner:
- Lentil stew with mixed vegetables (carrots, celery, onions).
- Brown rice or sweet potatoes.
Snacks:
- Fresh fruit, such as apple slices with almond butter.
- Raw veggies with hummus.
Meal Plan 2: Affordable Vegan Delights
Breakfast:
- Smoothie with frozen berries, spinach, banana, and almond milk.
- Whole-grain toast with avocado.
Lunch:
- Budget-friendly vegetable stir-fry with tofu and a soy-ginger sauce.
- Quinoa or brown rice.
Dinner:
- Spaghetti with tomato sauce and sautéed vegetables (use whole-grain or legume-based pasta).
- Side salad with mixed greens.
Snacks:
- Rice cakes with peanut butter.
- Fresh fruit, like orange slices.
Choosing a healthy plant-based and vegan diet is most beneficial when it comes to:
-
Higher levels of energy;
-
Improved sleep;
-
 Aids in energy and overall happiness;
Aids in energy and overall happiness; -
Provides a sense of comfort and relief;
-
Could prevent major diseases such as obesity and diabetes;
-
Accomplish weight-loss and management; and
-
Improves mental and cognitive functioning.
There are really no excuses not to try healthier habits in your everyday life. If you are a man or woman looking for specific benefits of adopting healthier habits or just want to know about the general healing properties of herbs. Please remember to comment or post any health questions, or contact us directly!