Craniofacial
anomalies also known as “CFAs” consist of a physical birth defect resulting in abnormal structures and underdevelopment affecting the bones, muscles, and tissues of the face and skull.
Many CFAs go overlooked due to the extensive lack of knowledge. Children and young adults with CFAs are at high risk for bullying, social rejection, and psychological distress, all of which are linked to detrimental health and developmental outcomes (Seehra et al., 2011).
Competency is a challenging issue in the fact that there are very few cases involving CFAs, and they are often ignored by providers in lieu of more common problems which can cause a scarcity of expertise.
The general lack of knowledge cause problematic barriers for medical professionals in diagnosing but even more so efficiently and adequately treating CFAs (Bemmels et al., 2013).
PROBLEM STATEMENT
Children and young adults born with CFAs often have concerns and social anxieties resultant from their physical appearance which ultimately can have a negative effect on their quality of life. CFAs are problematic and often have multiple areas of concern that necessitate comprehensive care and treatment from a collaborative medical team beginning early childhood. Technology and latest advances afford us with a variety of surgical options for patients with CFAs in obtaining reconstructive plastic surgery which is a complicated process in itself (Geirdal et al., 2015).
Having a child with a physical birth defect often affects the entire family, especially the parents. Parents are often not prepared in raising a child born with a CFAs. Therefore they often encounter unique challenges and in that they passionately seek to enhance their child’s life in any way possible, and in some cases inadvertently making poor decisions in selecting surgical care for their child. Some of the challenges we face today in dealing with CFAs is that there is a prevalent lack of education and awareness in the initial diagnosis and treatment stages of such disorders (Mathiesen et al., 2012).
PURPOSE OF THE STUDY
This qualitative study seeks in identifying and understanding the psychological and societal effects individuals with CFAs may experience. The purpose of this study is to consider statistical data and information with regards to the number of individuals with CFAs who suffer from psychological disorders resultant from either the lack of surgical care or consequences of surgical errors, along with a proposal for education and treatment.
If children and young adults with CFAs can be afforded with the best methods of treatment and surgical care, the chances of psychological disorders would greatly decline. However, many cases of CFAs can worsen after procedures such as reconstructive plastic surgery because of surgical errors in which other surgeons may attempt to try and repair despite uncertainties.
Sometimes the botched surgical circumstances are so severe that it is nearly impossible to seek to reconstruct the damage, but yet it is still done over and over again (Bemmels et al., 2013).
This focus of this study is to develop an understanding as to the necessity for reconstructive plastic surgery for those born with CFAs and if any psychological repercussions exist without. Furthermore, this study will focus on the consequences of surgical errors resulting in psychosocial outcomes and establish potential resolutions in efforts to eradicate or reduce the unintended consequences of botched reconstructive plastic surgery (Jenkinson et al., 2015).
RESEARCH QUESTIONS
Five core questions need to be addressed and detailed relating to the psychological impact of CFAs, the following research questions were explored:
- Most often the parents decide as to whether or not they will elect their child born with a CFA. When considering what is in “the child’s best interest” what does this mean in this context and from whose perspective?
- What type of psychosocial impact exists in regards to those born with CFAs?
- How can we better educate medical professionals, parents, and society at large in efforts to properly treat children and adults born with CFAs?
- How does the prevalence of consequences resultant of surgical errors affect individuals and families with CFAs?
- What are some resolutions in avoiding consequences of surgical mistakes?
HYPOTHESIS
It is hypothesized that there is a psychosocial impact with respects to physical appearance for individuals with CFAs. Additionally, it is hypothesized that individuals born with CFAs, in comparison to a general population sample, will have higher frequencies of depression, social anxieties, lower social competence – all of which can result in an adverse impact on their quality of life (Jenkinson et al., 2015).
THEORETICAL PERSPECTIVE
There is considerable literature regarding the correlation between psychosocial adjustment and stigmatization as to CFAs, which has been primarily from a theoretical perspective – which is supported by qualitative research through the utilization of the following methods:
- Cross-sectional survey assessments;
- Telephonic interviews;
- Previous studies accommodated for many demographical factors;
- Document review;
- Data analysis; and
- Individual observation of children and adults with CFA’s ages 12 to 61 years of age (Masnari et al., 2013).
LITERATURE REVIEW
According to research, physical birth defects affect approximately one in thirty-three children born in the U.S., and approximately one in four adults suffer from a psychological illness. While the rates of mental illness, in general, are high, they are also high for those born with CFAs. Additionally, research has shown that CFAs are amongst the most common birth defects and have significant practical, aesthetic, and societal repercussions.
While there are few cases where individuals sustain a craniofacial birth defect later in life due to injuries or disease, most cases of CFAs are often incurred at birth. Pursuant to research children born with CFAs may also suffer from a variety of medical issues involving their vision, hearing, or speech; which can be resultant of their CFA (Singh et al., 2015).
Research has established that CFAs can lead to various psychosocial development issues entailing of considerable social anxieties and avoidance attesting to interfere with the quality of life. Additionally, various studies have established that the adult population of those born with CFAs are at risk of developing psychosocial problems attributable to concerns relating to their facial appearance.
There is substantial and compelling literature on craniofacial abnormalities and the psychological and societal reactions and judgments. Such literature identifies a variety of subjective challenges and obstacles individuals with CFAs experience (Jenkinson et al., 2015).
Additionally, researchers have taken into consideration that the degree of the psychological effects of craniofacial abnormalities may not have a correlation as to the level of its genetic impact. However, studies have discovered a connection between CFAs and the increased reports and observations of behavioral issues at home and learning difficulties at school.
There are social stigmas and perceptions among the general population who have no ties to CFAs. It is widely assumed that children and young adults born with CFAs are also mentally challenged, especially if they require advanced hearing technology or speech therapy. While this has proven to be true in particular circumstances of CFAs, it is most certainly not true in all cases.
In fact, many children born with CFAs often have average intelligence (Masnari et al., 2013).
RESEARCH DESIGN AND METHODS
This is a qualitative study on the subject of psychosocial problems corresponding with adjustment as well as the necessity and benefits of reconstructive plastic surgery for individuals with CFAs. This study was conducted online and via telephone through various craniofacial communities, and twenty-five subjects were interviewed and observed for six weeks.
The data and information collected entails of a combination of previous studies accommodated for many demographical factors, interviews, survey, data analysis, and document review. Such information was obtained through the utilization of self-report surveys, in the format of written questionnaires and formally organized interviews in efforts to collect data information as to the backgrounds, behaviors, perspectives, and philosophies of a small to medium sized group participants with CFAs.
A grounded theory approach was utilized in efforts to enable the data collected to develop into new literature that may not have been considered before. This method utilizes foundation and presents the scope for imagination and creativity with the data in efforts to guide the study. This qualitative study focuses on elucidating personal experiences of children and adults with CFAs explaining their experiences and feelings in their own words.
Additionally, individual interviews were also conducted with medical professionals and parents of children with CFAs. This study utilized such methods in efforts to measure the psychosocial problems corresponding with adjustment as well as to develop an understanding as to the necessity for reconstructive plastic surgery and if any psychological repercussions exist without (Mathiesen et al., 2012).
PARTICIPANTS
The qualitative research design utilized a partially structured interview process with children and adults with CFA’s ages 12 to 61 years old, but also included parents and medical professionals. Interviews were conducted via telephone and online chat in a one-on-one setting and were recorded for more enhanced analysis purposes.
Every interview conducted lasted approximately thirty minutes to one hour. All of these interviews have been included in the data analysis; however, personal information will remain confidential, and there will be no direct quotations included from these interviews.
INDEPENDENT AND DEPENDENT VARIABLES
Evaluation measures involve the Quality of Life Questionnaire (TAPQOL), Perceived Stigmatization Questionnaire, Child Behavior Checklist (CBCL), and health-related quality of life (HRQOL). The independent variables in this study will include individual child characteristics which are a direct result of the CFAs and variables which represent the psychosocial development. Such CFA variables consist of; hearing capability, speech quality, and physical attractiveness.
Child psychosocial variables consist of; social skills, self-concept, externalizing behavioral issues, and, internalizing behavioral issues. While children with CFAs have not been identified to suffer from low self-perspective or psychological illness, however, it has been determined that they do exhibit patterns of increased societal reserve and self-consciousness concerning their physical appearance (Masnari et al., 2013).
DATA ANALYSIS
In this qualitative study, descriptive measurements were used in efforts to obtain an understanding of the data gathered from the surveys and interviews. Evaluation questionnaire tools and individual interviews were conducted and analyzed in efforts to determine if psychosocial adjustment problems were existent. Additionally, the cross-sectional study measured psychosocial adjustment and the HRQOL in children with CFAs and identified prospective conjectures of adjustment.
Findings have effects for the design of a potential correlational research study in efforts to examine the consequences of prolonged surgical intervention, establish qualitative analyses – which aim to understand parental perceptions concerning reconstructive craniofacial surgery for their children with CFAs, and studies of the manner in which surgical decisions are made and negotiated for, more specifically for children with CFAs and the reasoning on why (Mathiesen et al., 2012).
The data collected will be concluded along with the results of the completed questionnaires and interviews – all of which will be sent to a third-party contractor for a second opinion evaluation in efforts to avoid results based on research bias. The researchers will be accountable for implementing the results rendered by the third-party contractor in efforts to create a detailed analysis of findings and a retrospective chart assessment to examine the comprehensive set of dynamics as to the psychosocial impact of CFAs.
Results will be used towards future research studies, employing a correlational research study in efforts to obtain a comprehensive view of the psychosocial impact through the lifetime at each stage of development, affording opportunity for the results to be more applicable for clinical practice purposes. Additionally, such results from this study can serve as a substance to further inform and guide future research on the topic of the psychosocial impact of CFAs (Jenkinson et al., 2015).
ANTICIPATED RESULTS
As a consequence, it is anticipated that individuals with CFAs are at risk for psychosocial difficulties with untreated craniofacial abnormalities due to the lack of medically necessary surgical care or by the reasoning of distress resultant from surgical related errors and complications. Should this anticipation be correct, individuals with CFAs left untreated, commonly results in an adverse impact on; physical appearance, hearing, speech, as well as physical and psychological wellbeing.
For example, a female subject born with a CFA and in her late 20s, was interviewed, and she reported that her condition up until recently was left untreated, and she struggles tremendously in her speech capabilities, stating that she regularly has problems in simply interacting with others, especially young males (Bemmels et al., 2013).
CONCLUSION
It has been determined that children with CFAs often have been regarded as retaining usual self-perspective. However, they often experience psychosocial problems corresponding with adjustment. Psychosocial adjustment problems are identified by the development of psychological and/or behavioral symptoms such as; withdrawal, societal anxieties, depression, physical aggression, employment issues, academic difficulties, social conflicts or behavioral issues at home and school (Knight et al., 2015).
There have been a number of psychological risk factors in CFAs identified that could possibly damage a child’s psychological adjustment, most often attributable to parental overprotectiveness or guilt, consequently stigmatizing societal reactions to CFAs and particular neuropsychological circumstances notwithstanding that many children born with
CFAs seemingly retain common psychosocial development. However, the risk of developing learning impairments and disruptive behavioral disorders in this particular population group is greater than anticipated which implies that children born with CFAs would considerably benefit from psychological evaluation and treatment (Masnari et al., 2013).
It is of great significance that parents retain awareness as to the effect of CFAs and how they can have a negative effect on their child’s quality of life. Parents who lack education and awareness of CFAs often have communication issues from and with medical professionals.
Therefore many parents lack the ability to provide their child with the best medical care possible. Professional and parent education training is essential for parents to have a better understanding and position in caring and handling for their child born with a CFA (Mathiesen et al., 2012).
The results of this qualitative study have produced more questions than answers; There is an essential need for further empirical research and studies to be conducted on this subject matter for a clearer understanding and better resolution strategies. Such studies will allow us to understand the risks faced by those born with CFAs, early intervention and surgical treatment in efforts to lessen if not eradicate the possibility of psychosocial difficulties.
Being born with a craniofacial abnormality is a challenge and source of terrible emotional anguish that most cannot even remotely begin to identify with. People are a part of our everyday lives, going in and going out, and that will never change. We identify with others through social interaction, personal connection.
Our physical attributes are without a doubt our identities and what we all first take notice of when first meeting someone. We currently live in a day of age where physical appearance has become such a necessity of everyday life especially for many individuals who may lack education and/or understanding as to the harmful effects of societal judgment and bullying (Rose et al., 2013).
Regardless of the subjective feelings on this topic, reality is that many individuals with CFAs identify with others through the visualization of their faces. CFA subjects have often stated that they were forced in coming to terms with their physical disability and that they are inevitably and precisely what they see in the mirror, which is what others on the outside see too.
Thus, many individuals born with CFAs take drastic measures in hiding from society and social isolation through the means of numerous reconstructive surgeries in efforts to repair their facial disfigurement. The number of individuals born with and who have experienced suffering from the traumatizing terrors of outside judgment, bullying and self-judgement are very high (Romero-Maroto et al., 2015).
Without proper treatment consisting of craniofacial surgical intervention and psychological treatment, it is likely something that will follow them for the rest of their natural lives. While surgical intervention is often the most desirable approach to treating individuals with CFAs, however, it is essential for parents to make wise and medically necessary surgical decisions during childhood years, leaving them the choice to elect in making surgical decisions based on their own merits once adulthood is reached (Mathiesen et al., 2012).
Psychological Impact of Craniofacial Anomalies: An Annotated Bibliography
Singh, V. P., & Moss, T. P. (December 01, 2015). Psychological impact of visible differences in patients with congenital craniofacial anomalies. Progress in Orthodontics, 16, 1, 1-9.
The authors, researchers at the Department of Orthodontics and Dentofacial Orthopedics and Department of Health Psychology, conducted a study measuring the social and psychological effects of facial and dental appearance in patients suffering from craniofacial abnormalities in contrast to the general population.
Patients born with craniofacial abnormalities often have appearance-related concerns and are at risk for psychosocial difficulties. Facial appearance is considered as a significant need for healthy psychosocial development. There is a lack of qualitative research in the craniofacial field as it is rather contradictory and suffers various gaps for scientific reasons. These consist of contradiction in psychoanalysis scales and constructs used and the lack of legitimacy and reliability in many of the measurements.
Researchers emphasized the need to move from a ‘medical model’ towards a ‘social science model.’ Craniofacial abnormalities are facial disfigurements incurred at birth and can range in severity, however; research has established that craniofacial conditions can lead to various psychosocial development issues entailing of considerable social anxieties and avoidance – all of which can result in an adverse impact on their quality of life.
There are a variety of potential issues in the patient group of craniofacial abnormalities which are further complicated by an increased occurrence of malocclusion and dental anomalies. The best treatment method is multifaceted, which involves team collaboration and support from various specialties.
Throughout nearly all segments of treatment, dental services are necessary from an early age to late adult life. It is imperative for patients suffering from craniofacial abnormalities to have decent facial and dental appearance as it can have a constructive role on their self-esteem and psychological behavior.
Romero-Maroto, M., Santos-Puerta, N., González, O. M. J., & Peñacoba-Puente, C. (August 01, 2015). The Impact of Dental Appearance and Anxiety on Self-Esteem in Adult Orthodontic Patients. Orthodontics & Craniofacial Research, 18, 3, 143-155.
The authors, researchers from the Department of Orthodontics, Department of Psychology and Rey Juan Carlos University from Alcorcón, Madrid, Spain, conducted a study in efforts to evaluate the connection concerning different measurements as to the effects of dental appearance and self-esteem in adult patients undergoing orthodontic treatment.
The study had particularly emphasized the potential intervening role of anxiety and depression by conducting measurements as to the effect of dental appearance utilizing the Psychosocial Impact of Dental Aesthetics Questionnaire (PIDAQ). The PIDAQ provides exceptionally useful statistical information on aspects of oral health and oral health-related quality of life (OHRQoL). OHRQoL is a multifaceted construct that measures and documents the practical and psychosocial results of oral disorders.
A total of 85 adult patients were individually assigned to one of the two groups (experimental and control). Both groups established that self-esteem correlated with a number of negative outcomes with all measurements of dental appearance outcomes, not including the positive dental self-esteem measurement, which showed statistically significant positive correlations.
Anxiety was positively correlated with patients’ psychological impact, social influence, and appearance concerns while no statistically significant correlations were shown among dental self-esteem. However, in patients undergoing orthodontic treatment, anxiety was found to play an intervening role amongst dental impact measurements and self-esteem, whereas the control group found anxiety to play an intervening role concerning the psychological impact and self-esteem.
Anxiety serves as an essential role in the outcomes of perceived dental treatment effect on self-esteem in adult patients’ undergoing orthodontic treatment. Such results have proved as significant practical results for the objective of bio-psycho-social intervention programs that study cognitive and affective factors as a vital segment of orthodontic treatment in adults.
Jenkinson, E., Williamson, H., Byron-Daniel, J., & Moss, T. P. (October 16, 2015). Systematic Review: Psychosocial Interventions for Children and Young People with Visible Differences Resulting from Appearance Altering Conditions, Injury, or Treatment Effects. Journal of Pediatric Psychology, 40, 10, 1017-1033.
The authors, researchers from the Centre of Appearance Research, University of the West of England, conducted a study in efforts to assess the efficiencies of psychosocial interventions for children and adolescents with discernible facial differences with respects to improving self-confidence, social functioning, psychological health, and behavioral results analytically. Studies involved multiple appropriate databases and electronic sources, meeting prespecified appraisal and eligibility criteria, evaluated using methods that aim to minimize bias.
The studies utilized the Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist (PRISMA), a validated, evidence-based applied reporting and conducted instrument utilized as a basis for reporting systematic assessments of research, and in particular assessments of interventions.
Empirical research studies assessed the effectiveness of a residential social camps programs, social interaction skills training (SIST), behavioral therapy (BT), cognitive behavioral therapy (CBT), and physician-based assessment and counseling for exercise.
According to the American Camp Association residential camps help promote social interaction and self-efficacy among young adults who have special needs. SIST studies are conducted in efforts to assess the degree of social phobia and social anxiety as a result of disfigurement. BT and CBT are both scientifically established forms of psychotherapy that are effectual for various disorders and problems.
The reports in the studies retained a high and unclear risk of bias. Studies on residential social camps programs studies and physician-based assessment and counseling for exercise showed very little to no effect post-intervention with respects to self-confidence, social functioning, and psychological health. The five research studies assessing the effectiveness of SIST, CBT, and BT provided very limited support as to their level of efficiency.
In closing, the study is inconclusive and requires further research before strong conclusions can be established. Supporting and adequate evidence is necessary as any erroneous or misleading contextual factors may lead to incorrect conclusions. Further meticulous research utilizing proper conclusive measures in efforts to assess the efficiency of interventions for children and young adults with discernible facial differences is required.
Bemmels, H., Biesecker, B., Schmidt, J. L., Krokosky, A., Guidotti, R., & Sutton, E. J. (January 01, 2013). Psychological and Social Factors in Undergoing Reconstructive Surgery Among Individuals with Craniofacial Conditions: An Exploratory Study. The Cleft Palate-Craniofacial Journal: Official Publication of the American Cleft Palate-Craniofacial Association, 50, 2, 158-6
The authors, researchers from the Department of Educational Psychology, University of Minnesota, Minneapolis, Minnesota; conducted a study on reconstructive plastic surgery and its effectiveness in improving psychological health for children suffering from craniofacial anomalies.
Very few studies have investigated the difficulties of reconstructive plastic surgery beyond the physical uncertainties and risks consisting of: negative treatment outcomes, brain damage, infection, and sometimes even death. The objective of this subjective study is to recognize the social and psychological inferences that such interventions can have for patients suffering from craniofacial anomalies. The study involved a total of 38 individuals with various craniofacial disorders between the ages of 12 to 61.
All patient participants were selectively considered before recruitment in this study. The variety of patient participant viewpoints and experiences reveal the complication of reconstructive plastic surgery. Craniofacial surgeon teams involved in patient care play a vital role in advising patients as well as their parents on the subject of current treatment options and alternatives.
The social and psychological repercussions of reconstructive plastic surgery should be precisely communicated in efforts to help families consider the uncertainties and risks as to the benefits of reconstructive plastic surgery in an informative and expressive manner.
MY SURGICAL EXPERIENCES
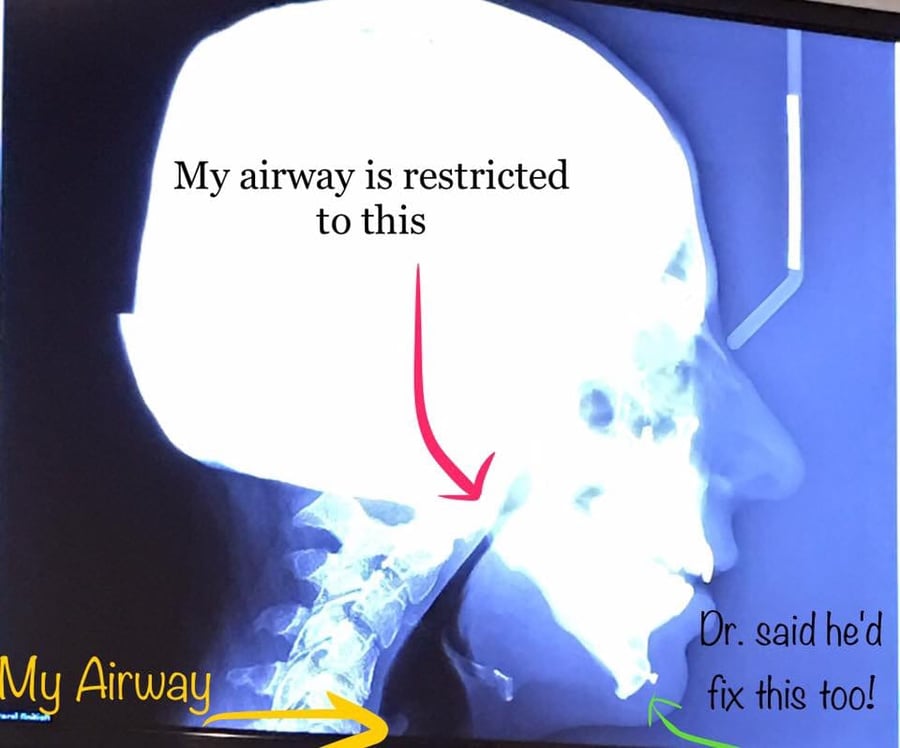
Craniofacial jaw surgery is excruciating and invasive. I can’t believe that I’m going through it a second time! There are others I’ve met in our community who’ve endured 5+ jaw surgeries if not more. I admire them for their tremendous strength!
Corrective Jaw Surgery Posted by Hashem Al-Ghaili on Wednesday, February 21, 2018
LOVE YOURSELF AND FIND YOUR NUTRITIONAL BALANCE. HEALTH IS TRULY YOUR GREATEST WEALTH.
I FOUND LOVE AND SO CAN YOU!


R.I.P. to my beautiful grandmother Mary that passed years ago before I had a chance to know her. Like me, she was born with Treacher Collins Syndrome. My biological father, brother, uncle, and many of my cousins were also born with this craniofacial condition.
CRANIOFACIAL STUDY BY UCLA DR. JUSTINE LEE
Were you or your child born with a craniofacial disorder? Join our online Facebook community to find upcoming Events and Gatherings near you.
References
Knight, J., Cassell, C. H., Meyer, R. E., & Strauss, R. P. (May 01, 2015). Academic Outcomes of Children With Isolated Orofacial Clefts Compared With Children Without a Major Birth Defect. The Cleft Palate-Craniofacial Journal, 52, 3, 259-268.
Geirdal, A. Ø., Saltnes, S. S., Storhaug, K., Åsten, P., Nordgarden, H., & Jensen, J. L. (April 01, 2015). Living with orofacial conditions: psychological distress and quality of life in adults affected with Treacher Collins syndrome, cherubism, or oligodontia/ectodermal dysplasia—a comparative study. Quality of Life Research : an International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation – Official Journal of the International Society of Quality of Life Research, 24, 4, 927-935.
Raquel Gonçalves Vieira-Andrade, & Saul Martins de Paiva and Leandro Silva Marques. (2015). Impact of Malocclusions on Quality of Life from Childhood to Adulthood. InT
Seehra, J., Newton, J. T., & DiBiase, A. T. (January 01, 2011). Bullying in school children – its relationship to dental appearance and psychosocial implications: an update for GDPs. British Dental Journal, 210, 9, 411-5.
Masnari, O., Schiestl, C., Rössler, J., Gütlein, S. K., Neuhaus, K., Weibel, L., Meuli, M., … Landolt, M. A. (January 01, 2013). Stigmatization predicts psychological adjustment and quality of life in children and adolescents with a facial difference. Journal of Pediatric Psychology, 38, 2, 162-72.
Mathiesen, A. M., Frost, C. J., Dent, K. M., & Feldkamp, M. L. (December 01, 2012). Parental Needs among Children with Birth Defects: Defining a Parent-to-Parent Support Network. Journal of Genetic Counseling, 21, 6, 862-872.